Full Answer
What is the Cy 2022 Medicare Physician Fee Schedule (PFS)?
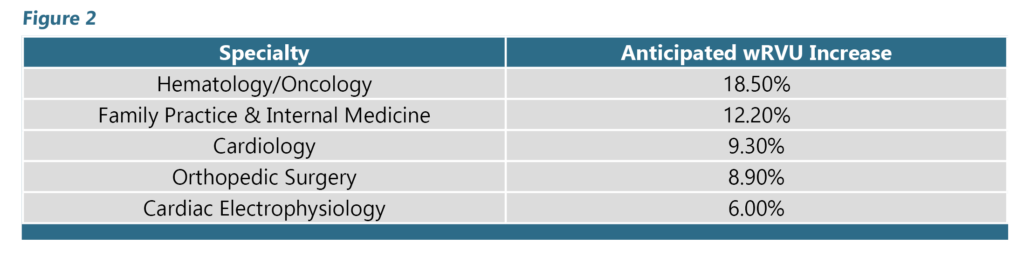
CMS issued the CY 2022 Medicare Physician Fee Schedule (PFS) final rule that updates payment policies, payment rates, and other provisions for services. See a summary of key provisions, effective on or after January 1, 2022:
How does Medicaid work in New Jersey?
NJ Medicaid & Managed Care In 1995, New Jersey Medicaid began moving Medicaid beneficiaries from a traditional fee-for-service health insurance program, in which healthcare providers bill Medicaid directly, into managed care.
What is the Medicare physician fee schedule proposed rule?
This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2021. This proposed rule proposes potentially misvalued codes and other policies affecting the calculation of payment rates.
When does the New Jersey Medicaid promoting interoperability program end?
All the participants for the New Jersey Medicaid Promoting Interoperability Program will now have until 11:59 pm ET on June 30, 2020. Click here for additional details related to the program update due to COVID-19 crisis.

Is NJ FamilyCare covered by Medicaid?
NJ FamilyCare It includes people who qualify for Children's Health Insurance Program (CHIP) or Medicaid. Eligibility for NJ FamilyCare is based on income and household size. Residents may enroll in NJ FamilyCare year round.
Does NJ Medicaid accept paper claims?
Paper claims and claims submitted through Direct Data Entry require both the prescriber's NPI and 7 digit NJ Medicaid provider number. Claims that do not provide this information or provide invalid information in this field are not being approved for payment.
Can you bill a Medicaid patient if you are not a participating provider in NJ?
MEDICAID HEALTH PLAN PROVIDERS ARE PROHIBITED FROM BILLING YOU FOR MEDICAID COVERED SERVICES. Please note: Medicare providers who do not participate with Medicaid have the right not to accept you as a patient. You must find Medicare providers who are willing to treat patients who have Medicare and Medicaid.
What is the timely filing limit for NJ Medicaid?
Timeframes are consistent with the New Jersey Division of Banking and Insurance (DOBI) for all medical services. Providers are to submit coordination of benefits (COB) claims within 60 days from the date of the primary insurer's explanation of benefits (EOB) or 180 days from the dates of service, whichever is later.
Does NJ Medicaid check your bank account?
While Medicaid agencies do not have independent access to a Medicaid recipient's financial statements, Medicaid does an annual update to make sure a Medicaid recipient still meets the financial eligibility requirements. Furthermore, a Medicaid agency can ask for bank statements at any time, not just on an annual basis.
What assets are exempt from Medicaid in New Jersey?
Exemptions include personal belongings, household furnishings, an automobile, irrevocable burial trusts, and generally one's primary home. For home exemption, the Medicaid applicant must live in the home or have intent to return, and in 2022, their home equity interest must be no greater than $955,000.
What is the difference between a participating and non-participating provider?
Participating Provider versus Non-Participating Provider - Reimbursement is 5 percent higher than the non-participating amount. - Medigap information is transferred. - A non-participating provider has not entered into an agreement to accept assignment on all Medicare claims.
Can doctors refuse Medicaid patients?
When uncovered costs become too great, physicians are ethically justified in refusing to accept Medicaid patients, according to Sade. “If they do accept such patients, however, they are ethically obligated to offer them the same care as they do for all of their patients,” Sade says.
Can we bill the patient if provider is out-of-network?
To truly bill on an out-of-network basis, one typically bills without checking off Accept Assignment. Second, you need to know if the patient has out-of-network benefits, and if so, if there are strings attached. For example, you may need to get prior approval from the carrier (i.e., precertification).
Do you have to renew Medicaid every year NJ?
You must fill out a Renewal Application every year to maintain your health care coverage. You can call NJ FamilyCare at 1-800-701-0710 (TTY 1-800-701-0720) to find out your renewal date or to ask for a renewal form.
What is Medicaid filing limit?
TIMELY FILING GUIDELINES Print Straight Medicaid claims must be filed within 12 months of the date of service. KIDMED claims must be filed within 60 days from the date of service.
Does NJ Medicaid automatically renew?
If you have NJ FamilyCare or Medicaid, you must renew every 12 months and stay current with any premium you owe. Those who do not renew their eligibility or do not pay their premiums on time will lose their benefits with Horizon NJ Health. Certain members will not be able to reenroll.
Where do I mail NJ Medicaid claims?
Claim appeals may be submitted by:Fax: 973-522-4678.Mail: Horizon NJ Health. Claim Appeals. P.O. Box 63000. Newark, NJ 07101-8064.
Can you submit Medicare claims on paper?
The Administrative Simplification Compliance Act (ASCA) requires that Medicare claims be sent electronically unless certain exceptions are met. Providers meeting an ASCA exception may send their claims to Medicare on a paper claim form.
Can you bill Medicare paper claims?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
What are two types of paper claims submitted for health services?
The two most common claim forms are the CMS-1500 and the UB-04. The UB-04 (CMS 1450) is a claim form used by hospitals, nursing facilities, in-patient, and other facility providers. A specific facility provider of service may also utilize this type of form.
What is NJ Medicaid?
NJ Medicaid. Medicaid provides health insurance to parents/caretakers and dependent children, pregnant women, and people who are aged, blind or disabled. These programs pay for hospital services, doctor visits, prescriptions, nursing home care and other healthcare needs, depending on what program a person is eligible for.
What department administers home and community-based programs for seniors?
The Division of Aging Services in the Department of Human Services administers a number of Home and Community-Based Programs for seniors.
Does New Jersey have medicaid?
Within New Jersey Medicaid there are also a number of special programs designed to meet the specific medical needs of certain groups of people who would not otherwise qualify for the program. These include:
How much is the ACA application fee for 2021?
New: Notice of Application Fee: The Patient Protection Affordable Care Act, better known as the Affordable Care Act (ACA), has implemented a $599.00 application fee (for calendar year (CY) 2021) to be paid by a list of defined new provider types applying to NJ Medicaid/NJ FamilyCare, for those applicable provider types that are required to be re-enrolled (revalidated) and for those providers who wish to have their files reactivated.This required fee will apply to the following applicants: ambulatory care clinics, ambulatory surgical centers, federally qualified health centers (FQHC), ESRD centers, independent laboratories, mental health clinics, Medicare-certified home care agencies (only), hospice agencies, hospitals, long-term care (LTC) facilities, medical suppliers, optical appliance providers, pharmacies, portable x-ray providers, prosthetic and orthotic (P&O) providers, rehabilitation providers, special hospitals, intermediate care facilities (ICF/IID), workfirst providers, and ambulance transportation providers. Please note: submitting proof (eg. copy of a cancelled check) that an application fee already was paid to Medicare or another state’s Medicaid agency when applying or re-enrolling will waive the required application fee.
What is NJFC fillable pdf?
This fillable pdf is available to individuals requesting temporary enrollment in the NJFC Program, including State managed care providers who would otherwise submit the 21st Century Cures Act application. The fillable pdf is not intended for use by hospitals. Facilities may be required to supply additional information on request.
How to report Medicaid fraud?
Click here To Report Fraud or Abuse In the Medicaid Program or Call 1-888-937-2835.
When do you need to enter a new email address for NJMMIS?
Users will be prompted to enter a new email address when no email address is on file with Gainwell Technologies before being allowed to access the NJMMIS.
How to contact the provider enrollment unit?
If you have any questions, please contact the Provider Enrollment Unit at 609-588-6036.
When was the HMO encounters system guide revised?
Revised: A revised HMO Encounters Systems Guide dated October 2021 has been published and made available in the Forms & Documents link at the left of the page or it can be found under the HIPAA Companion Guides paragraph under the additional Headlines page or click here.
When was the HIPAA 837 updated?
Revised: A revised 837/835/277P HIPAA Companion Guide dated November 2021 has been published and made available in the Forms & Documents link at the left of the page or it can be found under the HIPAA Companion Guides paragraph under additional Headlines page or click here.
When will Medicare start charging for PFS 2022?
The CY 2022 Medicare Physician Fee Schedule Proposed Rule with comment period was placed on display at the Federal Register on July 13, 2021. This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2022.
When is the Medicare Physician Fee Schedule 2020?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
What is the MPFS conversion factor for 2021?
CMS has recalculated the MPFS payment rates and conversion factor to reflect these changes. The revised MPFS conversion factor for CY 2021 is 34.8931. The revised payment rates are available in the Downloads section of the CY 2021 Physician Fee Schedule final rule (CMS-1734-F) webpage.
What is the calendar year 2021 PFS?
The calendar year (CY) 2021 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
What is the CY 2021 rule?
The calendar year (CY) 2021 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When will CMS issue a correction notice for 2021?
On January 19, 2021, CMS issued a correction notice to the Calendar Year 2021 PFS Final Rule published on December 28, 2020, and a subsequent correcting amendment on February 16, 2021. On March 18, 2021, CMS issued an additional correction notice to the Calendar Year 2021 PFS Final Rule. These notices can be viewed at the following link:
What is the 2020 PFS rule?
The calendar year (CY) 2020 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
