Does Aetna have a good dental plan?
The Aetna Dental Direct plan covers preventative care 100% with no out of pocket cost. And you don’t have to have Aetna medical or other coverage with us to purchase. While most dental plans require a waiting period for major services like crowns or root canals, if you switch from your existing comparable plan to an Aetna plan, we will waive the waiting period.
How much does Aetna dental insurance cost?
The premium for two family members is $148.53 while it is at $217.56 for every family with three or more members. For Aetna Dental, the charge for an individual plan is at $139.95 per annum while a family plan costs $179.95.
What is Aetna PPO dental plan?
This Aetna Dental® Preferred Provider Organization (PPO) benefits summary is provided by Aetna Life Insurance Company for some of the more frequently performed dental procedures. Under this plan, you may choose at the time of service either a PPO participating dentist or any nonparticipating dentist.
Do dentists offer payment plans?
Fortunately, many dentists offer the option of a payment plan, so instead of paying one giant sum, patients can pay in smaller increments over time. There are different payment plans and different ways to arrange payment with your dentist. Here we explain how dental payment plans work and what to be aware of before you sign up for one.

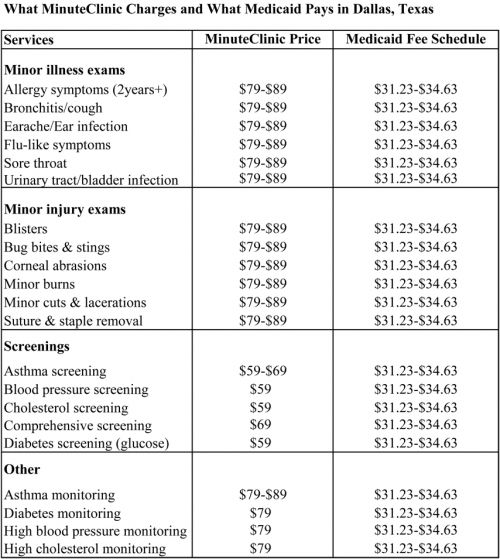
What is a fee schedule?
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
Does Aetna accept consult codes 2022?
Starting March 1, 2022, we will no longer pay office consultation codes 99241, 99242, 99243, 99244 and 99245.
How do I get my Aetna EOB?
You can view, print or download your EOB and other documents anytime at www.aetna.com. Want to stop the paper? It's easy. Log in to your secure member website at www.aetna.com, go to “Your Profile,” provide a valid email address and select your paper-saving preferences.
Does Aetna follow CMS guidelines?
Providers are required to comply with CMS coding and billing requirements. For a provider who treats commercial or Medicaid members, we will pay for covered services in accordance with the member's health plan benefits and applicable laws and regulations.
Is CPT code 99244 a valid code?
The Current Procedural Terminology (CPT®) code 99244 as maintained by American Medical Association, is a medical procedural code under the range - New or Established Patient Office or Other Outpatient Consultation Services.
Does CPT code 99244 need a modifier?
I looked up your codes on CCI Edits and it shows that the 99214/99244 would require a -59 modifier to "unbundle" it from the 95970.
What is Aetna EOB?
Explanation of Benefits (EOB) - This is not a bill. This statement is called your EOB. It shows how much you may owe, the amount that was billed, and your member rate. It also shows the amount you saved and what your plan paid.
How do you know your EOB?
How to read your EOBProvider—The name of the doctor or specialist who provided the service.Service/Procedure—The type of service you received.Total Cost—The amount we pay for the service. ... Not Covered—The amount of the service not covered (this usually only occurs if the service is denied).More items...
What is included in the EOB?
EOB means Explanation of Benefits. It is a statement from your health insurance company providing details on payment for a medical service you received and explains what portion of those services were paid by your insurance plan and what part you're responsible for paying.
What is the CMS factor for 2022?
$34.6062On Dec. 16, the Centers for Medicare and Medicaid Services (CMS) announced an updated 2022 physician fee schedule conversion factor of $34.6062, according to McDermott+Consulting.
Does Aetna require preauthorization?
Your clinical team or PCP requests prior authorization before the service is rendered. You do not need a referral or prior authorization to get emergency services. Aetna providers follow prior authorization guidelines.
Is Aetna Medicare or Medicaid?
Aetna offers Medicaid insurance plans in many states. Aetna also runs Children's Health Insurance Plan (CHIP), Medicare Advantage, behavioral health and long-term care programs in some states. Our plans have different names in different states, but all offer the same high-quality care.
Does Aetna take consult codes?
Starting March 1, 2022, we will no longer pay office consultation codes 99241, 99242, 99243, 99244 and 99245.
Does Cigna accept consult codes?
Cigna does not reimburse for: For outpatient or inpatient consult codes.
What is the CPT code for hospital consultation?
Consultations for Medicare patients are reported with new patient (99201–99205) or established patient (99212–99215) Current Procedural Terminology (CPT) codes. For non-Medicare patients (unless otherwise instructed by a payor), office or other outpatient consultations are reported with codes 99241– 99245.
What modifier does Aetna use for telemedicine?
Telemedicine coding, billing and rates For commercial members non-facility telemedicine claims must use POS 02 or POS 10 with the GT or 95 modifier.
How long does it take to pay a DME claim?
Within fifteen (15) days, pay the electronic DME clean claim or notify the provider or designee that the claim is denied or contested. The notification to the provider of a contested claim must include an itemized list of denial reasons or codes and additional information or documents necessary to process the claim.
How to claim DME?
Providers submitting claims for Durable Medical Equipment (DME) Rental should use CMS 1500 Form. DME rental claims are only paid up to the purchase price of the durable medical equipment. Units billed for Medicaid equal the amount of days billed. Since appropriate billing for CMS is 1 Unit per month, in order to determine the amount of days needed to determine appropriate benefits payable under Medicaid, the claim requires the date span (from and to date) of the rental. Medicaid will calculate the amount of days needed for the claim based on the date span. Appropriate modifier, RR, is required for all rentals.
What is prior authorization in ABHFL?
Prior Authorization is needed for requests greater than limits indicated on Fee Schedule.
Does Aetna reimburse DME?
Aetna Better Health bases reimbursement of Durable Medical Equipment (DME) services on the Agency’s fee schedules. Any code that doesn’t have an assigned rate requires prior authorization and will be reimbursed at the manufacturer’s invoice plus 15%.
Do you need authorization for DME?
Standard limits do not apply, authorization is required for all DME services. Authorization is based on a member's individual needs as assessed on their care plan.
Who must sign a document and plan of care?
Documentation and Plan of Care must be signed by/dated by physician with specific term, duration & diagnosis
Does Aetna cover wheelchairs?
Aetna Better Health covers customized wheelchairs for children and adults as listed in the DME and Medical Supply Services Coverage and Limitations Handbook, pages 2-91 through 2-96, and the DME and Medical Supply Services Fee Schedule, including all accompanying parts needed to operate the equipment. Prior authorization is required.
