When is the Medicare Physician Fee Schedule 2020?
When will Medicare start charging for PFS 2022?
What is the MPFS conversion factor for 2021?
What is the calendar year 2021 PFS?
What is the CY 2021 rule?
When will CMS issue a correction notice for 2021?
What is the 2020 PFS rule?
See 4 more
About this website
Is the 2022 Medicare physician fee schedule available?
The Centers for Medicare & Medicaid Services (CMS) released the 2022 Medicare Physician Fee Schedule and Quality Payment Program final rule on Nov. 2 .
Where can I download the Medicare physician fee schedule?
you may wish to access the Medicare Physician Fee Schedule Database (MPFSDB)/Relative Value File on the CMS website. CMS offers the complete file in several different formats and provides a single code look up. Access the Medicare Physician Fee Schedule Database (MPFSDB)/Relative Value File on the CMS website.
What is the Medicare physician fee schedule?
The Medicare Physician Fee Schedule (MPFS) is the annual regulatory rule released by the Centers for Medicare and Medicaid Services (CMS) that updates the standards for physician reimbursement and policies related to the delivery of health care.
What is the Medicare fee for 2022?
(Your state will pay the standard premium amount of $170.10 in 2022.) If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard Part B premium and an income-related monthly adjustment amount.
How Much Does Medicare pay for a 99214?
$141.78CPT Code 99214 Reimbursement Rate Medicare reimburses for procedure code 99214 at $141.78.
How often is the Medicare fee schedule updated?
annuallyThe fee schedule is updated annually by the Centers for Medicare and Medicaid Services (CMS) with new rates going into effect January 1 of each year. By law, CMS must publish the new rates in the Federal Register by November of the preceding year.
How do I find the Medicare allowable rate?
You can search the MPFS on the federal Medicare website to find out the Medicare reimbursement rate for specific services, treatments or devices. Simply enter the HCPCS code and click “Search fees” to view Medicare's reimbursement rate for the given service or item.
Did Medicare reimbursement go down in 2022?
Scheduled Payment Reductions to 2022 Medicare Physician Fee Schedule. Absent congressional action, a 9.75% cut was scheduled to take effect Jan. 1, 2022. *Congress has reduced 3% of the scheduled 3.75% cut to the Medicare Physician fee schedule conversion factor.
What is the maximum fee a Medicare participating provider can collect for services?
They can charge up to 15% over the Medicare-approved amount for a service, but no more than that. This is called "the limiting charge."
What are the Medicare changes for 2022?
Higher Medicare Part B costs The cost of Medicare Part B will go from $148.50 per month in 2021 to $170.10 per month in 2022, an increase of $21.60 per month. The Medicare Part B deductible is also rising in 2022. The annual Part B deductible will go from $203 in 2021 to $233 in 2022, an increase of $30.
Are Medicare premiums going up in 2022?
In November 2021, CMS announced that the Part B standard monthly premium increased from $148.50 in 2021 to $170.10 in 2022. This increase was driven in part by the statutory requirement to prepare for potential expenses, such as spending trends driven by COVID-19 and uncertain pricing and utilization of Aduhelm™.
How much will Medicare premiums increase in 2022?
California Health Advocates > Prescription Drugs - Blog > Why Did Medicare's Part B Premium Rise 14.5% in 2022? If you're on Medicare, chances are you had a bit of a shock when seeing the 2022 Medicare Part B premium amount. It went up by $21.60, from $148.50 in 2021 to $170.10 in 2022.
What is the physician look up tool?
This look-up tool is a searchable database that allows you to look up a provider by National Provider Identifier (NPI), or by name and location. The look-up tool will return information on services and procedures provided to beneficiaries enrolled in Original Medicare (fee-for-service) for 2020.
Is the 2020 Medicare fee schedule available?
The Centers for Medicare and Medicaid Services (CMS) has released the 2020 Medicare Physician Fee Schedule final rule addressing Medicare payment and quality provisions for physicians in 2020.
How are RBRVS fee schedules calculated?
Payments are calculated by multiplying the combined costs of a service times a conversion factor (a monetary amount determined by CMS) and adjusting for geographical differences in resource costs.
What is a reimbursement schedule?
Reimbursement Schedule means the compensation payable to Practitioner by a Payor, as payment in full, for Practitioner's provision of Covered Services to Members.
Calendar Year (CY) 2022 Medicare Physician Fee Schedule Proposed Rule
On July 13, 2021, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule that announces and solicits public comments on proposed policy changes for Medicare payments under the Physician Fee Schedule (PFS), and other Medicare Part B issues, on or after January 1, 2022.
Calendar Year (CY) 2022 Medicare Physician Fee Schedule Final Rule
On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) issued a final rule that includes updates on policy changes for Medicare payments under the Physician Fee Schedule (PFS), and other Medicare Part B issues, on or after January 1, 2022.
Fee Schedule Lookup - NGSMEDICARE
Fee Schedule Assistance. The fee schedule assistance page provides access to information about fee schedule definitions and acronyms.. National Fee Schedules. Access the CMS website to view and download the following national fee schedules:. Ambulance Fee Schedule; Ambulatory Surgical Center (ASC) Payment; Clinical Laboratory Fee Schedule
2022 Medicare Physician Fee Schedules (MPFS)
By continuing, you agree to follow our policies to protect your identity. This means you won’t share your user ID, password, or other identity credentials. It also means you won’t use a computer program to bypass our CAPTCHA security check.
Fee schedule data files - fcso.com
This website provides information and news about the Medicare program for health care professionals only.All communication and issues regarding your Medicare benefits are handled directly by Medicare and not through this website. For the most comprehensive experience, we encourage you to visit Medicare.gov or call 1-800-MEDICARE. In the event your provider fails to submit your Medicare claim ...
When is the Medicare Physician Fee Schedule 2020?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
When will Medicare start charging for PFS 2022?
The CY 2022 Medicare Physician Fee Schedule Proposed Rule with comment period was placed on display at the Federal Register on July 13, 2021. This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2022.
What is the MPFS conversion factor for 2021?
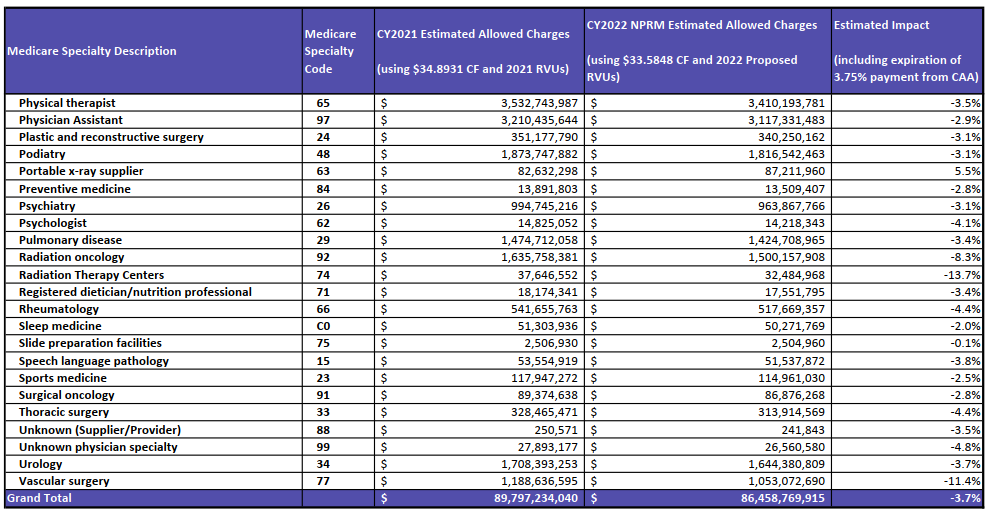
CMS has recalculated the MPFS payment rates and conversion factor to reflect these changes. The revised MPFS conversion factor for CY 2021 is 34.8931. The revised payment rates are available in the Downloads section of the CY 2021 Physician Fee Schedule final rule (CMS-1734-F) webpage.
What is the calendar year 2021 PFS?
The calendar year (CY) 2021 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
What is the CY 2021 rule?
The calendar year (CY) 2021 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When will CMS issue a correction notice for 2021?
On January 19, 2021, CMS issued a correction notice to the Calendar Year 2021 PFS Final Rule published on December 28, 2020, and a subsequent correcting amendment on February 16, 2021. On March 18, 2021, CMS issued an additional correction notice to the Calendar Year 2021 PFS Final Rule. These notices can be viewed at the following link:
What is the 2020 PFS rule?
The calendar year (CY) 2020 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
What is the calendar year 2022 PFS?
The calendar year (CY) 2022 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a health care system that results in better accessibility, quality, affordability, empowerment, and innovation.
What is the PFS conversion factor for 2021?
With the proposed budget neutrality adjustment to account for changes in RVUs (required by law), and expiration of the 3.75 percent payment increase provided for CY 2021 by the Consolidated Appropriations Act, 2021 (CAA), the proposed CY 2022 PFS conversion factor is $33.58, a decrease of $1.31 from the CY 2021 PFS conversion factor of $34.89. The PFS conversion factor reflects the statutory update of 0.00 percent and the adjustment necessary to account for changes in relative value units and expenditures that would result from our proposed policies.
What is the OIG methodology for Medicare?
Section 405 of the CAA requires the Office of Inspector General (OIG) to conduct periodic studies on non-covered, self-administered versions of drugs or biologicals that are included in the calculation of payment under section 1847A of the Social Security Act. This provision permits CMS to apply a payment limit calculation methodology (the “lesser of” methodology) to applicable billing codes, if deemed appropriate. That is, the Medicare payment limit for the drug or biological billing code would be the lesser of: (1) the payment limit determined using the current methodology (where the calculation includes the ASPs of the self-administered versions), or (2) the payment limit calculated after excluding the non-covered, self-administered versions. CMS is proposing the “lesser of” methodology for drug and biological products that may be identified by future OIG reports.
When will telehealth services be added to the Medicare telehealth list?
As CMS continues to evaluate the temporary expansion of telehealth services that were added to the telehealth list during the COVID-19 PHE, CMS is proposing to allow certain services added to the Medicare telehealth list to remain on the list to the end of December 31, 2023, so that there is a glide path to evaluate whether the services should be permanently added to the telehealth list following the COVID-19 PHE.
How long after hospitalization can you get pulmonary rehabilitation?
We are proposing to expand coverage of outpatient pulmonary rehabilitation services, paid under Medicare Part B, to beneficiaries who were hospitalized with COVID-19 and experience persistent symptoms, including respiratory dysfunction, for at least four weeks after hospitalization.
When is telehealth required in CAA?
Section 123 of the CAA removed the geographic restrictions and added the home of the beneficiary as a permissible originating site for telehealth services when used for the purposes of diagnosis, evaluation, or treatment of a mental health disorder, and requires that there be an in-person, non-telehealth service with the physician or practitioner within six months prior to the initial telehealth service, and thereafter, at intervals as specified by the Secretary.
Why do you need to report modifiers on a claim?
Requiring reporting of a modifier on the claim to help ensure program integrity.
Congressional Response to Medicare Payment Crisis
CMS implemented this change in response to the Protecting Medicare and American Farmers from Sequester Cuts Act, which was signed into law by President Biden on Dec. 10, 2021.
Scheduled Payment Reductions to 2022 Medicare Physician Fee Schedule
Absent congressional action, a 9.75% cut was scheduled to take effect Jan. 1, 2022.
When are MPFS fees due for 2020?
The CY 2020 MPFS fees have been updated by the Further Consolidated Appropriations Act of 2020. The fees are valid January 1, 2020 through December 31, 2020
What is limiting charge 2021?
2021. If you have elected to be a participant during 2021, the limiting charges indicated on the report will not pertain to your practice. The non-participating fee schedule amounts and limiting charges do not apply to services or supplies unless they are paid under the physician fee schedule.
What is Medicare Part B?
Medicare Part B pays for physician services based on the Medicare Physician Fee Schedule (MPFS), which lists the more than 7,400 unique covered services and their payment rates. Physicians' services include office visits, surgical procedures, anesthesia services and a range of other diagnostic and therapeutic services.
What is a non-facility practice expense?
The higher non-facility practice expense RVUs are generally used to calculate payments for services performed in a physician's office and for services furnished to a patient in the patient's home; facility; or institution other than a hospital, skilled nursing facility (SNF), or ambulatory surgical center (ASC). For these services, the physician typically bears the cost of resources, such as labor, medical supplies and medical equipment associated with the physician's service.
Do you have to accept assignment for Medicare?
Some practitioners who provide services under the Medicare program are required to accept assignment for all Medicare claims for their services. This means that they must accept the Medicare allowed charge amount as payment in full for their practitioner services. The beneficiary's liability is limited to any applicable deductible plus the 20 percent coinsurance. The following practitioners must accept assignment for all Medicare covered services they furnish, and carriers do not send a participation enrollment package to these practitioners. The non-participating fee schedule amounts and limiting charges do not apply to services rendered by:
Is facility based fee a separate RVU?
The facility-based fees are linked to their own separate RVUs independent of the non-facility fee RVUs. This differs from the former site-of-service fee reductions, which were based simply on a percentage reduction of the full fee rather than a separate RVU.
Do limiting charges apply to Medicare?
If you have elected to be a participant during 2020, the limiting charges indicated on the report will not pertain to your practice. The non-participating fee schedule amounts and limiting charges do not apply to services or supplies unless they are paid under the physician fee schedule. Limiting charge applies to unassigned claims by non-participating providers. All services provided to Medicare beneficiaries are subject to audit and documentation requirements.
When is the Medicare Physician Fee Schedule 2020?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
When will Medicare start charging for PFS 2022?
The CY 2022 Medicare Physician Fee Schedule Proposed Rule with comment period was placed on display at the Federal Register on July 13, 2021. This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2022.
What is the MPFS conversion factor for 2021?
CMS has recalculated the MPFS payment rates and conversion factor to reflect these changes. The revised MPFS conversion factor for CY 2021 is 34.8931. The revised payment rates are available in the Downloads section of the CY 2021 Physician Fee Schedule final rule (CMS-1734-F) webpage.
What is the calendar year 2021 PFS?
The calendar year (CY) 2021 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
What is the CY 2021 rule?
The calendar year (CY) 2021 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When will CMS issue a correction notice for 2021?
On January 19, 2021, CMS issued a correction notice to the Calendar Year 2021 PFS Final Rule published on December 28, 2020, and a subsequent correcting amendment on February 16, 2021. On March 18, 2021, CMS issued an additional correction notice to the Calendar Year 2021 PFS Final Rule. These notices can be viewed at the following link:
What is the 2020 PFS rule?
The calendar year (CY) 2020 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
